Abstract
Background: Annual transcranial doppler (TCD) screening is strongly recommended for patients with sickle cell anemia (SCA) between the ages of 2 to 16 years to identify children at highest risk for stroke. Implementation of this screening and treating identified patients with chronic transfusion has decreased the incidence of overt stroke. Nonetheless, adherence to TCD screening guidelines is poor and many children with SCA do not receive an annual TCD.
The purpose of this study is to evaluate adherence to TCD screening among a cohort of patients with SCA seen in the emergency department (ED) for an acute problem. Previous work has demonstrated that SCD-related outpatient visits are important "missed opportunities" for TCD screening. We hypothesized that ED encounters also represent potential opportunities to identify patients in need of TCD screening who do not attend clinic regularly.
Methods: We conducted a retrospective chart review of the medical records of all patients with sickle cell disease (SCD) seen in the ED at a large, urban pediatric institution between February 2016 and April 2017. Patients were identified using an ED clinical registry that includes all ED patient encounters. We excluded patients who do not need TCD screening (sickle cell disease genotypes other than SS and Sβ0 thalassemia, age <2 or >16 years, on chronic transfusions, history of hematopoietic stem cell transplant). We also excluded patients documented to previously have inadequate TCD bone windows and patients who did not receive their regular hematology care at the study institution. For eligible patients who had multiple ED encounters during the study period, data was extracted at the time of the first ED encounter during the study period.
Eligible patients who had received a TCD in the last year (adherent to TCD screening) were compared to patients who had not received a TCD in the last year (nonadherent to TCD screening). Categorical data was analyzed with the chi-square test. Continuous data was analyzed using the two-sample t-test. P value of <0.05 was considered statistically significant.
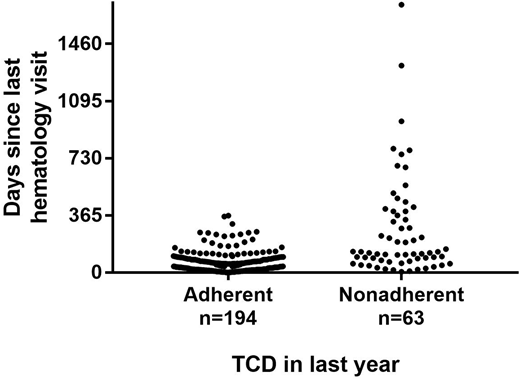
Results: During the 64 week study period, 739 patients with SCD were seen in the ED. A total of 482 patients were excluded for the following reasons: non-SCA genotype (n=164), age (n=139), followed at outside institution (n=129), chronic transfusion (n=38), prior TCD window problem (n=10), history of transplant (n=2); leaving 257 patients with SCA aged 2-16 years for study. Among this study group, 63 patients (25%) had not received a needed TCD in the last year, including 19 patients (7%) who had never had a TCD. When excluding patients aged 2-2.99 years (n=33) in whom a first TCD may have been planned soon after the ED encounter, a similar proportion of patients still had not received a TCD in the last year (53/224, 24%) but a slightly smaller proportion had never had a TCD (9/224, 4%). Patient age and sex were not associated with TCD screening adherence (p>0.7). Patients adherent to TCD screening were more likely to be taking hydroxyurea (67% vs. 29%, p<0.0001). A recent hematology clinic visit was significantly associated with TCD screening adherence. All patients adherent to TCD screening had a clinic visit in the last year compared to 75% of nonadherent patients, p<0.0001. The mean interval time since the last hematology clinic appointment from the ED encounter was greater for TCD nonadherent patients, 70 vs. 270 days p<0.0001 (Figure).
Conclusion: Patients with SCA who present to the ED and are nonadherent to TCD screening guidelines are less likely to have had a recent hematology clinic visit. Therefore, the ED may be an important location for identifying patients lost to regular clinic follow-up in need of a TCD. An intervention that specifically targets this patient population will likely improve TCD screening rates and stroke prevention.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.